The article below is by DSC. Read the original article here.
On September 14th, NDIS Minister Bill Shorten released details of a new operational plan to reduce hospital discharge delays for NDIS participants.
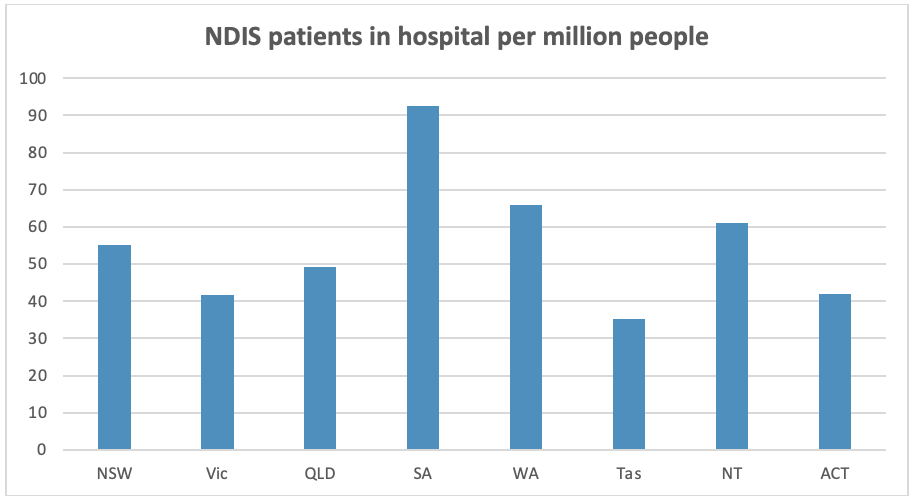
The data shows that a new strategy is urgently needed. On average, people on the NDIS are waiting 160 days for supports to be put in place to allow them to safely leave hospital. Many of these people have no medical reason to remain in hospital. According to Crikey, 1,834 of the 2,328 NDIS participants in hospital right now are medically ready for discharge, that’s 59%. The situation differs slightly by state and territory. Data provided to the ABC show that South Australia and Western Australia have the highest number of NDIS participants in hospital on a per capita basis.
Few people want to spend a day longer in hospital than absolutely necessary, let alone 160 days. So it is undeniably bad outcome for the people directly affected. It’s also expensive, with these hospital stays costing at least $2,000 a night and by some estimates $1bn a year. Moreover, the backlog takes up hospital beds in the middle of a public health crisis.
Shorten has said the delays are probably caused by several factors, including the snail’s pace of our bureaucracy, a lack of appropriate support and accommodation, and poor communication between hospitals and other departments.
The new operational plan aims to address these issues by:
- The NDIA approving an NDIS hospital discharge plan within 30 days. Our understanding is that an NDIS hospital discharge plan is an updated NDIS plan that includes the supports a person needs to safely leave hospital. But few details were provided in the press release.
- The NDIA contacting NDIS participants within four days of admission to hospital.
- Increasing the number of hospital liaison officers from 33 to 40 by the end of September 2022. That’s a 20% increase in the number of staff within about 2 weeks of the announcement.
- Improving staff training and streamlining processes for faster decision making.
- Improving data collection to monitor progress over time.
Implementing this plan will require cooperation between the Commonwealth and the states and territories that manage the hospital systems. Traditionally, these relationships have been more than a tad tense. In the lead-up to the announcement, Shorten told The Australian that he believes states and territories need to do more to support people with disability.
You can read the full press release here: https://ministers.dss.gov.au/media-releases/9106.


